The 2nd Peking University International Narrative Medicine Conference Successfully Held in Beijing
From November 15 to 16, 2025, the 2nd Peking University International Narrative Medicine Conference was grandly held in Beijing. With the theme of “Building Consensuses, Advocating Practices”, the conference aimed to further consolidate consensus on the evolutionary landscape of narrative medicine and promote the optimal practice paths for medical humanities, health humanities, and narrative medicine. Gathering the wisdom of researchers at home and abroad, the conference shared cutting-edge theories and latest practical achievements in the field, conducted cross-cultural dialogues from a global perspective, and jointly mapped out the future development direction of narrative medicine.
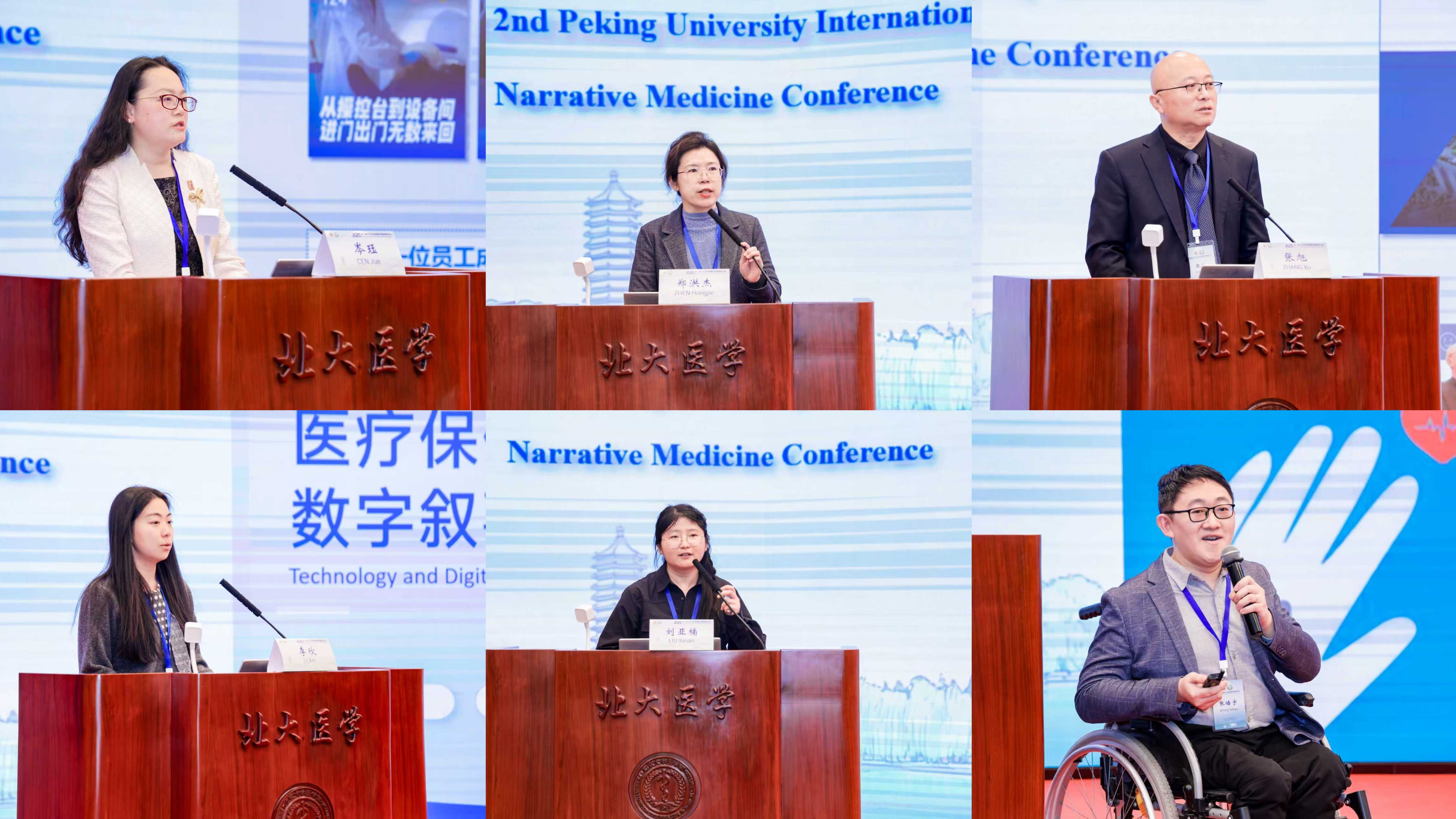
The conference featured two plenary sessions and nine parallel sessions. More than 100 renowned experts and young scholars from North America, Europe, Oceania, Asia, and China delivered academic presentations, and over 260 attendees came from institutions of higher education, research institutes, medical institutions, etc., including some patient representatives deeply involved in narrative medicine practice, who jointly witnessed this academic feast.

On the morning of November 15, the opening ceremony and the first half of the plenary presentations were hosted by Guo Liping, Dean of the School of Health Humanities, Peking University. Xu Changshun, Level II Bureau Rank Official of the Beijing Municipal Health Commission, attended the opening ceremony and delivered a speech. He pointed out that since its birth, narrative medicine has provided a crucial pathway to address the imbalance between medical technologization and humanism in modern medicine, and has become an effective tool for the implementation of medical humanistic spirit. Focusing on the transition of narrative medicine from “shared knowledge” to “joint action”, he shared three insights : “Gaining knowledge through practice”, “Putting knowledge into practice”, and “Unifying knowledge and practice”. In addition, he introduced the pilot achievements of 22 municipal hospitals in Beijing in building humanistic departments through narrative medicine, and stated clearly that efforts will be made to promote narrative medicine from “shared knowledge” to “joint action” in the hospital system through institutional guarantees and platform construction.

In the first half of the plenary presentations, Professor Wang Yifang from the School of Health Humanities, Peking University, delivered a report titled “Three Pairs of Categories in Narrative Medicine”, emphasizing that narrative medicine is not only a new cognitive paradigm but also an innovative clinical path. He focused on analyzing three key pairs of categories—narrative medicine and evidence-based medicine, narrative medicine and narrative nursing, modern medical narrative and traditional Chinese medicine (TCM) narrative—stressing that clarifying the connotation of concepts is crucial for advancing the discipline. Professor Wang Yifang pointed out that different cognitive paradigms should not simply “seek common ground while reserving differences” but rather “reflect on changes through differences”, achieving interaction and harmony in clinical practice through the interweaving of perspectives.
Shang Hongcai, Dean of Dongfang Hospital, Beijing University of Chinese Medicine, delivered a report titled “Approaches and Methods for Integrating Narrative Medicine and Evidence-Based Medicine”. He pointed out that current evidence-based practice still fall short in addressing “patient values”, while narrative medicine can effectively bridge the gap between evidence-based treatment and medical humanities. He proposed a dual-track approach of “evidence-based narrative medicine” and “narrative-based evidence-based medicine.” This includes conducting clinical research on narrative interventions, enhancing physicians’ narrative competence, and integrating narrative thinking into the construction of evidence ecosystems, thereby offering new directions for advancing medical research and service capabilities.
Professor Ge Lun from Beijing University of Civil Engineering and Architecture delivered a report titled “On the Theory and Design Methodology of Narrative Evidence-Based Design (NEBD) — A Case Study of Gansu Maternal and Child Healthcare Hospital.” Using Gansu Maternal and Child Health Hospital as a case study, she elaborated on how to transform patients’ experiences and stories into concrete spatial needs and create healing environments through architectural language. This research fills the cognitive gap in understanding narrative medicine within architectural and spatial dimensions, providing theoretical support and practical examples for building humanistic healthcare environments.
The second half of the symposium was chaired by Chen Xuyan, Vice Dean of Tsinghua Medicine, Tsinghua University. Professor Frances Kam Yuet Wong from the School of Nursing, Hong Kong Polytechnic University delivered a report titled “Importance of Parental Involvement in Pediatric Palliative Care in Hong Kong: A Qualitative Case Study”, exploring the significance of parental involvement in pediatric palliative care in Hong Kong. The study compared the perceptions of care needs among pediatric patients, parents, and healthcare providers, revealing that while their concerns overlapped, their perspectives differed significantly: healthcare providers focused more on medical issues, while families prioritized daily life challenges. She emphasized that integrating multiple voices and promoting shared decision-making are crucial for bridging service gaps and achieving holistic care.
The conference released three consensus documents jointly formulated by Professor Guo Liping and her team from the School of Health Humanities, Peking University, Deputy Director Zhu Liming and his team from Zhejiang Provincial Hospital Management Center, and Associate Professor Li Fei and her team from the School of Humanities and Social Sciences, Chinese Academy of Medical Sciences/Peking Union Medical College. Professor Guo Liping released the “Expert Consensus on the Construction of Humanized-care-oriented Clinical Departments in Medical Institutions in China (2025)”, Deputy Director Zhu Liming released the “Expert Consensus on the Practice of Narrative Medicine in Hospitals in China (2025)”, and Associate Professor Li Fei released the “Expert Consensus on Narrative Medicine Education and Teaching in Medical Universities and Schools in China(2025) ”. These three expert consensuses construct the theoretical and practical system of narrative medicine practice in China from multiple dimensions such as the construction of humanistic departments, narrative medicine practice in hospitals, and narrative medicine education in medical colleges and universities. This marks a significant step forward in the standardization and systematization of narrative medicine in China.
Professor Emeritus Lennard J. Davis from the University of Illinois at Chicago delivered an online speech. From a cultural criticism perspective, he explored the interplay of biological and cultural factors within narratives of obsessive-compulsive disorder (OCD), revealing the latent power of historical context in understanding and healing the condition.
On the afternoon of November 15, Parallel Session 1 focused on the theoretical construction and clinical practice of TCM narrative medicine. Scholars present explained the multiple values of narrative medicine in patient rehabilitation and optimized diagnosis and treatment through classic texts such as “Guo Lin’s Diary”; from a holistic perspective, they constructed a narrative practice framework integrating the concept of harmony between man and nature and systematic ecology; at the clinical level, they established an evidence-based narrative model combining traditional Chinese and Western medicine, and extracted core narrative elements such as disease evolution and emotional factors. The scholars also explored contemporary relevance of traditional close reading methods, developing a TCM narrative theory system that synthesizes symbolic thinking with pattern differentiation and treatment. These explorations highlight the high consistency between TCM’s “people-oriented” concept and narrative medicine, providing important enlightenment for promoting the innovative development of medical humanities.

Parallel Session 2 focused on the clinical application of narrative medicine in fields such as cancer care, chronic disease and rare disease management. Through constructing the theoretical framework of “narrative palliative care” and combining in-depth interviews with colorectal cancer patients and osteogenesis imperfecta groups, participating scholars revealed the dynamic characteristics of patients’ disease cognition and psychological needs. They also carried out specific practical explorations such as the “human-shaped poster” nursing rounds model and narrative nursing experiments for diabetic patients, which improved the quality and warmth of clinical nursing. These studies highlight the core concept of elevating nursing from disease management to life care. By establishing emotional alliances and participating in patient story interpretation, they provide actionable pathways and methods for advancing medical humanism practices.

Parallel Session 3 focused on the practical application of narrative medicine in fields such as pain management, palliative care, and cross-cultural healthcare. Scholars demonstrated how narrative interventions help patients accept pain, alleviate anxiety and depression, and regulate fear. They also clarified how narrative nursing in palliative care not only enhances nurses’ competencies but also supports patients in achieving a dignified passing. Additionally, scholars examined the influence of cultural backgrounds on healthcare-seeking behaviors, explored the narrative value of “silence,” and discussed the role of narrative medicine in supporting evidence-based decision-making. These studies highlight the multidimensional value of narrative medicine in deepening doctor-patient understanding and optimizing clinical practice.

Parallel Session 4 focused on the diversified interdisciplinary practices of narrative medicine. Presentations by participating scholars spanned multiple dimensions such as literature, media, film and television, and education. They analyzed medical narratives and perspectives on life from a literary viewpoint, reflected on moral construction during public crises through media case studies, and explored trauma and healing through Brazilian indigenous cinema and Chinese-language films on dementia. Meanwhile, the localized “literature-clinic” intervention model grounded in systematic thinking, alongside comparative bibliometric studies across Chinese and international literature, collectively demonstrated narrative medicine’s immense potential in bridging literature and clinical practice, the individual and society, and local and global contexts, providing profound enlightenment for expanding the practice path of medical humanities.

Parallel Session 5 focused on the cutting-edge applications and ethical challenges of narrative medicine in diverse scenarios such as pediatrics, special education, and artificial intelligence(AI). Scholars conducted discussions from multiple dimensions including linguistics, philosophy, and clinical practice, covering topics such as the emotional construction of guardians’ discourse in pediatric medical complaints, the game between medical and educational discourse in special education, and the role and regulation of AI as a “narrative agent” in clinical decision-making. Concurrently, participants examined pivotal topics including the “cyborgization” experience of cochlear implant recipients, suicide motivation analysis among incapacitated elderly in care facilities, and how documentary narratives can reshape positive perceptions of aging. These discussions vividly demonstrated narrative medicine’s interdisciplinary vitality in addressing complex real-world challenges, opening new theoretical and ethical horizons for medical humanities practice.

On the morning of November 16, the first half of the conference program was chaired by Professor Guan Ruiyuan, Assistant Dean of the School of Health Humanities, Peking University. Maria Giulia Marini, President of the European Narrative Medicine Society (EUNAMES), delivered a report titled “Binary Stars of Meaning and Evidence: Bridging Narrative Medicine and Evidence-Based Medicine”. She noted that while evidence-based medicine is indispensable, researchers often misinterpret statistical probability as certainty. Narrative medicine, she emphasized, is key to addressing this gap. By integrating patient stories into clinical evidence through mixed research methods, she argued, we can build more humanistic healthcare practices.

Yoshiyuki Yama, Professor and Dean of the School of Human Well-being, Kwansei Gakuin University, delivered a report titled “The Role of Narrative in the Quality of Life (QOL) and Health of Older Adults: Insights from the Practice of Philosophy Café Activities at a Japanese Senior Welfare Centee”. He shared Japan's practice of promoting elderly social participation and improving their quality of life through “philosophy café” activities in the context of a super-aging society. He pointed out that narrative serves not only as a communication tool but also as a vital means to combat social isolation and maintain physical and mental well-being.
The second half of the conference was moderated by Assistant Professor Huang Rong from the School of Health Humanities, Peking University. Claire Hooker, Associate Professor of Health and Medical Humanities at Sydney Health Ethics, delivered a report titled “Grace Under Pressure: Changing Healthcare Culture Using Verbatim Theatre”, introducing how to use “verbatim theatre” to transform healthcare workplace culture. Through the play “Grace Under Pressure” and its supporting workshops, she demonstrated the remarkable effect of artistic intervention in improving medical staff’s communication and workplace behavior, providing an innovative path for improving the global healthcare workplace culture.
Jürgen Pieters, Director of the Ghent-based international research network CHARM, delivered a report titled “Taking Tolstoy to the Doctor: What If Ivan Ilyich Was Your Patient?”. He demonstrated how he used Tolstoy’s novel “The Death of Ivan Ilyich” as teaching material to discuss language and communication strategies in doctor-patient relationships with internal medicine residents. He emphasized that narrative medicine does not oppose biomedicine but complements it, jointly constructing a more complete medical landscape.
Penelope Scott, Associate Professor in Linguistics at the Department of Applied Linguistics, Xi’an Jiaotong-Liverpool University (XJTLU), delivered a report titled “Illness Metaphors in AI Art Creation: A Health Humanities Perspective”. She explored the potential and limitations of illness metaphors in visual narratives from the standpoint of AI-driven artistic creation. Scott noted that while AI image generation can assist patients in expressing pain that is hard to verbalize, caution is warranted regarding the metaphorical frameworks it may impose.
On the afternoon of November 16, Parallel Session 1 focused on the innovative applications of narrative medicine across multiple domains, including clinical practice, health promotion, and medical education. The research of participating scholars covered practical paths such as building emotional bonds among blood donors through two-way narrative exchange, realizing the reconstruction of disease meaning with intangible cultural heritage (ICH) techniques, and promoting the internalization of medical staff’s humanistic literacy through lunchtime book clubs. Participants also explored topics including pregnant women’s fear of childbirth, empathy development for nursing interns, and collaborative educational models across three learning settings, proposing actionable intervention and educational strategies. Their research underscored narrative medicine’s potential for integrating clinical care, cultural enrichment, and technological empowerment, providing dual theoretical and practical foundations for its systematic advancement.

Parallel Session 2 focused on the diversified practices and remarkable effects of narrative medicine interventions in various clinical fields. Scholars discussed how narrative medicine effectively enhances communication quality between general practitioners and patients, how holiday-themed narrative interventions improve disease understanding and quality of life for chronic illness patients, and how narrative medicine interventions improve hospitalization outcomes for neurosurgical patients and deepen understanding of disease in terminally ill children. They also delved into how interventions like music-based narratives provide emotional regulation and expression pathways for cancer patients and psychological rehabilitation. Their research shows the broad prospect of narrative medicine in improving doctor-patient relationships in palliative care scenarios and its in-depth integration with evidence-based medicine.

Parallel Session 3 focused on the application of narrative medicine in hospital management scenarios. Scholars discussed the significance of narrative medicine in effectively optimizing medical service processes and improving nursing levels. They also explored the application paths of narrative medicine from the perspectives of integrating medicine and art to inject humanistic warmth into hospitals, discussing digital narratives and technological ethics to provide new ideas for intelligent medical care, and reconstructing doctor-patient relationships by transforming patients’ subject roles. These explorations fully demonstrate that narrative medicine is promoting the high-quality development of medical services from multiple dimensions, realizing the dual improvement of technical efficiency and humanistic warmth.
Parallel Session 4 focused on the connections between narrative medicine and institutional identity, literature, and art. Through specific cases, scholars explored the ethical dilemmas of relative diagnosis and treatment in cross-cultural contexts, and how institutional narratives shape the identity of medical organizations. Through analyses of themes such as heart disease, disability, and maternal pain, they also revealed the intertwined relationship between the body and culture in illness narratives, demonstrating literature and art’s immense potential to counter social stigma and express personal and racial trauma. These studies collectively indicate that narrative medicine is constantly deepening the humanistic understanding of pain, trauma, and healing through ethical reflection, cultural criticism, and artistic practice.

The successful convening of this International Narrative Medicine Conference has consolidated consensus in the field of narrative medicine research and presented its rich and diverse practical pathways. Experts and scholars from around the world engaged in in-depth dialogues, and through the collision and integration of multiple perspectives, they have opened up broad space for further exploration of the theoretical framework and clinical pathways of narrative medicine. The conference released three expert consensuses, effectively promoting the standardization and systematization of narrative medicine practice in China, and providing valuable theoretical and practical resources for enhancing medical humanism. In the future, the Peking University School of Medical Humanities will continue organizing high-quality academic conferences, thoroughly implementing the “Healthcare Humanism Enhancement Action Plan (2024-2027)”, and fully supporting the implementation of the Healthy China Strategy.
During the conference, the award ceremony for the 3rd “The Warmth of Medicine” Essay Symposium was also held. Attendees included nationally renowned writer Bi Shumin, along with representatives from NEJM Frontiers in Medicine, Peking University School of Health Humanities, and the Taikang Yicai Public Welfare Foundation.


